The advances in the understanding of the biology of wound healing and periodontal regenerative technologies are applied to improve long-term clinical outcomes of teeth which are periodontally compromised by intrabony or inert-radicular defects.
 Periodontal regeneration is selected to:
Periodontal regeneration is selected to:
1. Increase the periodontal attachment of a compromised tooth.
2. Decrease in deep pockets to a more maintainable range.
3. Reduce the vertical and horizontal components of furcation defects.
There are different types of defects: suprabony (horizontal) defects, infrabony (vertical) defects and inter-radicular (furcation) defects. Suprabony defects are those where the base of the pocket is coronal to the alveolar crest. Infrabony defects are those who affect primary one tooth or a crater in which two adjacent root surfaces to a similar extent are affected. Acording to their morfology these defects are classified in terms of the residual bony walls, width of the defect (radiographic angel), and the extension around the tooth (three, two or one wall).
The diagnosis of the presence and the morphology of periodontal osseous lesions represent a major clinical challenge. It is done by a combination between clinical information and intraoral radiographs.
Etiology of the intrabony pocket involved tooth anatomy and tooth position. Tooth anatomy concerns with grooves, crevice or concavity on the root surface which facilitates accumulation of plaque and calculus formation, contact areas morphology, and also type of tooth. Tooth position which contributes to food impaction, plaque accumulation, angular position, or position of the tooth in respect to the alveolar housing and buccal bone are the local environmental factors which can initiate the infrabony pocket process. Another important factor in the etiology of the intrabony pocket is the occlusal traumatic lesion. Even though occlusal traumatism cannot cause pocket formation alone, as the pocket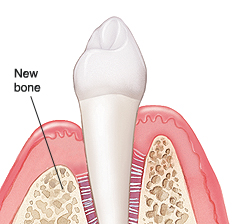 formation began with the local factors (calculus, food impaction), the occlusal trauma can affect the attachment apparatus. Local factors and traumatic occlusion will inevitably lead to the formation of intrabony pocket.
formation began with the local factors (calculus, food impaction), the occlusal trauma can affect the attachment apparatus. Local factors and traumatic occlusion will inevitably lead to the formation of intrabony pocket.
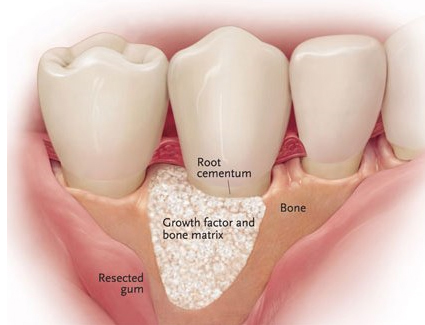
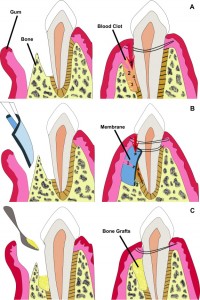
To fill the infrabony defects different types of bone grafts can be used. The autologous (bone harvested from the patient’s own body); allograft (cadaveric bone usually obtained from a bone bank); or synthetic. The success of this bone graft includes osteoconduction, osteoinduction, and osteogenesis (only occurs with autografts). Recent studies demonstrate that there is no significant difference between using an autologous and using allografts. The difference is that if autologous is used, there will be two surgical sites, so recovery becomes more painful. What really matters is to fill the intrabony defect with a graft to avoid a major problem.
By Prisma Dental
For more information contact Prisma Dental at their website. Prisma Dental Website